Minimally invasive cardiac procedures are revolutionizing the treatment of heart conditions, offering effective solutions with reduced recovery times, fewer complications, and improved patient experiences. By using catheter-based techniques, advanced imaging, and innovative devices, cardiologists can now perform complex interventions without the need for traditional open-heart surgery, making life-saving treatments accessible to a wider range of patients.
One of the most transformative procedures is Transcatheter Aortic Valve Replacement (TAVR). This technique allows patients with aortic stenosis — a condition where the heart’s aortic valve narrows — to avoid open-heart surgery. Using a catheter-based approach, physicians can implant replacement valves with precision, reducing procedural risk and improving outcomes. TAVR is especially beneficial for high-risk or elderly patients, providing enhanced quality of life, shorter hospital stays, and improved survival rates.
Leadless Pacemakers: Innovation in Cardiac Pacing
Leadless pacemakers represent another significant advancement. Unlike traditional pacemakers that require leads (wires) connecting the device to the heart, leadless pacemakers are tiny, self-contained devices implanted directly into the heart. This design minimizes infection risks, reduces complications, and allows for a quicker, more comfortable recovery. Patients experience efficient cardiac pacing without the discomfort and restrictions often associated with conventional pacemakers.


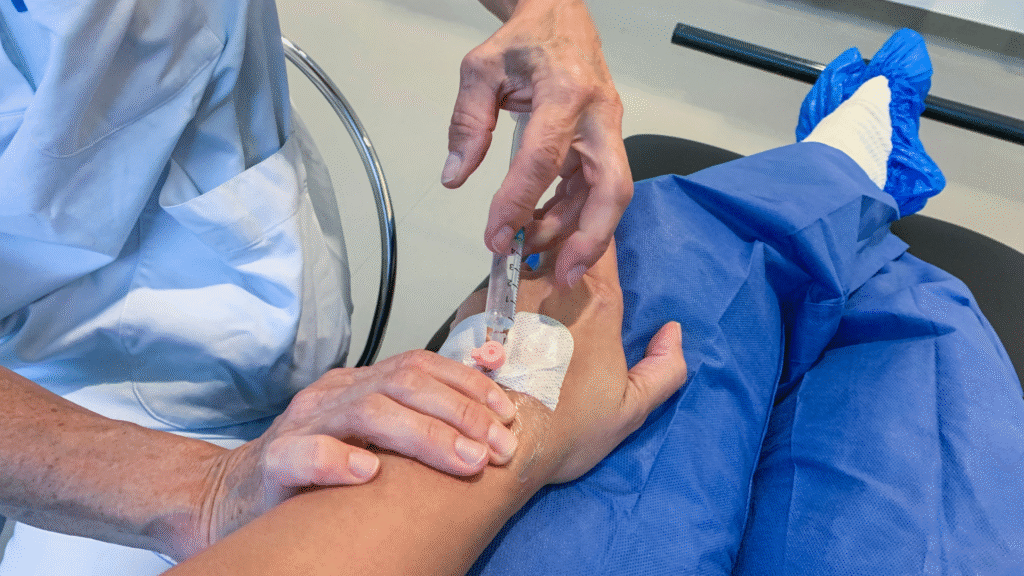
Percutaneous coronary interventions (PCI), including balloon angioplasty and stent placement, enable rapid treatment of narrowed or blocked arteries. These procedures restore blood flow efficiently, relieving symptoms such as chest pain and reducing the risk of heart attacks. Compared to open-heart bypass surgery, PCI offers shorter hospital stays, faster recovery, and quicker return to daily activities, making it a preferred option for many patients.
The success of minimally invasive procedures is enhanced by cutting-edge imaging technologies. 3D echocardiography, intraoperative guidance systems, and real-time fluoroscopy provide precise visualization of cardiac structures, allowing cardiologists to target specific areas accurately. This precision improves outcomes, reduces procedural risks, and ensures that interventions are tailored to each patient’s anatomy.
Minimally invasive cardiac procedures are particularly valuable for elderly patients or those with multiple comorbidities who may not tolerate traditional surgery. By reducing procedural stress, hospital stays, and complications, these techniques expand access to critical treatments, offering hope to patients who might otherwise have limited options.
Minimally invasive techniques are not just about smaller incisions — they are about giving patients a faster path back to life.
Patient Education and Post-Procedural Care
Patient education plays a crucial role in the success of minimally invasive interventions. Comprehensive guidance on pre-procedure preparation, post-procedure care, lifestyle adjustments, and cardiac rehabilitation ensures safer recovery and improved long-term outcomes. Engaged and informed patients are better equipped to follow medical advice and achieve optimal health results.
As medical technology continues to evolve, minimally invasive cardiac procedures are poised for further breakthroughs. Innovations in device design, imaging systems, robotic assistance, and procedural techniques will continue to enhance safety, precision, and patient comfort. Collectively, these advancements are transforming cardiovascular care, offering better long-term results, reduced risks, and improved quality of life for patients worldwide.


